Aetna Waiving Copays For Telehealth
Cost share waivers for any in-network covered medical or behavioral health services telemedicine visit for Aetna Student Health plans are extended until September 30, 2020. Medicare Advantage will continue to waive cost shares for in-network primary care and specialist telehealth visits, including outpatient behavioral and mental health. Aetna self-insured plan sponsors may waive these benefits at their discretion. Free COVID-19 testing We’ll waive the cost for testing, provided you meet the Centers for Disease Control and Prevention (CDC) guidelines for testing and your doctor requests it.
- Is Medicare Waiving Copays For Telemedicine
- Is Aetna Still Waiving Copays For Telehealth Visits
- Aetna Waiving Copays For Telehealth Providers
Several commercial health insurers will waive member cost-sharing — which includes copays, deductibles and coinsurance — for COVID-19 testing and treatment into the next year.
Aetna will cover appropriate evaluation and management codes with a wellness diagnosis for those aspects of the visit done via telehealth. Preventative visit codes should be reserved for such time when routine in-office visits resume and the remaining parts of the well visit can be completed. Aetna is here for you during the coronavirus (COVID-19) pandemic, no matter what. Learn about extra benefits and well-being resources just for you, find testing locations, get answers to the most frequently asked questions regarding COVID-19 and tips to stay safe, and much more.
Here are 14 commercial payers that have announced extensions to their COVID-19 cost-sharing waivers into 2021, per America's Health Insurance Plans. As of Dec. 2, the federal public health emergency period is scheduled to end Jan. 21, so many of the policies below also end on that day.
Editor's note: Policies vary by insurer. This list will be updated if more announcements are made. Email mhaefner@beckershealthcare.com if your company has implemented similar measures.
1. Aetna is waiving member cost-sharing for inpatient admissions to treat COVID-19 for commercially insured and Medicare Advantage members through Jan. 31.
2. Arkansas Blue Cross and Blue Shield expanded COVID-19-related benefits for fully insured and individual health plans through Jan. 21.
3. Playstation 4 app download pc. Avera Health Plans will waive cost-sharing for COVID-19 treatment with in-network providers through Jan. 21.
4. Blue Cross and Blue Shield of Kansas City will waive cost-sharing and copayments for COVID-19 inpatient hospital admissions through Jan. 20.
5. Blue Cross Blue Shield of Michigan and Blue Care Network will continue to waive cost-sharing for members who are diagnosed and treated for COVID-19 through March 31.
6. Blue Cross and Blue Shield of Minnesota is extending its cost-sharing waiver for in-network COVID-19 treatment through March 31.
7. Blue Cross and Blue Shield of Nebraska will waive cost-sharing for in-network COVID-19 testing and related services through Jan. 20.
8. Blue Cross and Blue Shield of North Carolina is extending its cost-sharing waiver for COVID-19 treatment through March 31.
9. Capital Blue Cross is waiving cost-sharing for provider visits that result in a COVID-19 test through Jan. 21.
10. Cigna is waiving out-of-pocket costs for COVID-19 visits with in-network providers through Jan. 21.
11. Premera Blue Cross is extending cost-sharing waivers for COVID-19 treatment through March 31 for both inpatient and outpatient treatment.
Is Medicare Waiving Copays For Telemedicine
12. Priority Health will waive cost-sharing for medically necessary treatment of COVID-19 through March 31.
13. QualChoice Health Insurance has waived cost-sharing payments for telehealth visits, and no pre-authorization is required through Jan. 21.
14. Security Health Plan is covering inpatient and observation treatment related to COVID-19 at 100 percent through Jan. 21.
More articles on payers:
UnitedHealthcare delays coding changes for lab tests
New Jersey school board sues Horizon, says insurer threatened to stop paying claims for 14,000 workers
18 payer exec moves in November
© Copyright ASC COMMUNICATIONS 2021. Interested in LINKING to or REPRINTING this content? View our policies by clicking here.
Is Aetna Still Waiving Copays For Telehealth Visits
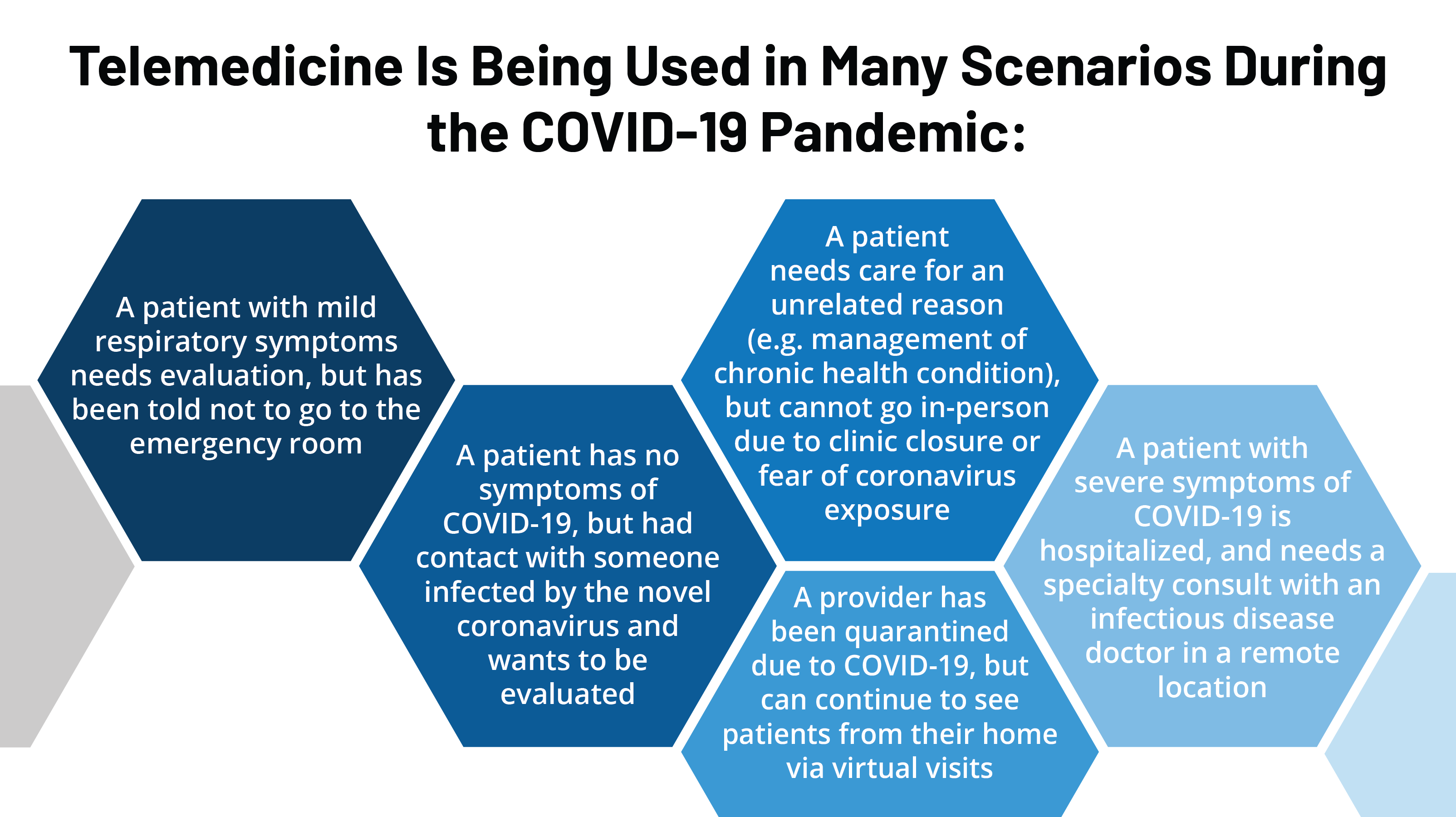
In light of the COVID-19 pandemic, many commercial health insurers waived cost-sharing for medical and behavioral telehealth services.
Becker's asked five of the largest for-profit insurers — Aetna, Anthem, Cigna, Humana and UnitedHealthcare — when those waivers are set to end.
Here's the projected expiration date of their telehealth cost waivers, as of Sept. 17. For reference, the current national public emergency health period — which was extended effective July 25 — is slated to end in late October, around the 23rd. If the PHE is extended again, some of the dates may be pushed backed.
Aetna
- Cost-share waivers for commercial telemedicine behavioral health services: Dec. 31
- Cost-share waivers for all Medicare telemedicine services: Dec. 31
Anthem
- Cost-share waivers for COVID-19 testing and related telehealth visits and telephonic-only visits: When PHE ends (around Oct. 23)
- Cost-share waivers for COVID-19 treatment from in-network providers accessed via telehealth: Dec. 31
- Cost-share waivers for non-COVID-19 telehealth visits across fully-insured employer and individual plans: Sept. 30
- Cost-share waivers for non-COVID-19 telehealth visits across Medicare and Medicaid plans: Dec. 31 (where not covered under a state program)
Cigna
- Cost-share waivers for COVID-19 telehealth visits across Medicare Advantage plans: Dec. 31
- Cost-share waivers for telehealth screenings for COVID-19 across commercial and individual/family plans: Oct. 31
- Cost-share waivers for non-COVID-19 in-network medical or behavioral telehealth visits across Medicare Advantage plans: Dec. 31
- Cost-share waivers for in-network virtual primary care and specialist office exams or consultations for non-COVID-19 care across individual/family plans: Oct. 31
- Expanded virtual medical care access for non-COVID-19 services from physicians and certain providers for commercial members: Dec. 31

Humana

- Cost-share waivers for all telehealth visits (primary, speciality and behavioral services) with in-network providers, regardless of COVID-19 diagnosis: Dec. 31
UnitedHealthcare
- Cost-share waivers and expanded access for COVID-19-related telehealth visits: Oct. 22
- Cost-share waivers and expanded access for non-COVID-19 telehealth visits with in-network providers: Sept. 30
Aetna Waiving Copays For Telehealth Providers
More article on payers:
Hackensack Meridian, RWJBarnabas, Horizon launch insurance company
CMS proposes payment changes to Medicare Advantage, Part D: 5 things to know
MedStar, CareFirst: New partnership to curb costs by $400M
© Copyright ASC COMMUNICATIONS 2021. Interested in LINKING to or REPRINTING this content? View our policies by clicking here.

